Pulmonary Embolism
PE diagnosis:
Hemodynamic Classification of Acute PE (AHA)
Massive PE
SBP <90 for 15 min or req. inopressor support
OR Pulselessness
OR Sustained HR <40, s/sx of shock
Submassive PE
SBP > 90 with evidence of RV dysfunction or myocardial necrosis. Specifically:
RV dilation (RVdiameter/LVdiameter > 0.9) on echo or CT
RV systolic dysfunction
BNP > 90 pg/mL or N-terminal pro-BNP > 500 pg/mL
EKG Δ's (RBBB, anteroseptal ST Δ's, anteroseptal TWI)
Troponin leak (Ti > 0.4 or Tt > 0.1)
Low-risk PE
Absence of above
Consider sending home if sPESI = 0
Simplified Pulmonary Embolism Severity Index:
Age > 80
History of cancer
Chronic cardiopulmonary disease
Pulse > 110
SBP < 100
SpO2 < 90% (requiring oxygen)
More on Submassive PE
Massive PE Physiology
(Oren Friedman lecture)
-RV spiral of death (to the right)
First thing that happens is a pressure load, mPAP increases exponentially
RV CANNOT HANDLE THIS PRESSURE LOAD like the LV can
If RV CO falls, LV CO falls too. They are both in series (preload) and in parallel (interventricular dependance)
Second thing is ischemia
RV is VERY sensitive to changes in coronary perfusion pressure
RV can become ischemic even with nrml coronaries
RVSP is essentially equal to PASP; RV perfusion pressure = Ao-PA pressures (see below)
RV is perfused through systole and diastole
If PA pressure (and thus RV pressure) > Ao pressure, RV ischemia!
RV ischemia = RV CO drop = RV pressure buildup.. vicious cycle
Hemodynamic MGMT in Massive PE
-Goal 1: Decrease PVR; first thing is HOW CAN I GET RID OF CLOT
Approach
Clinical assessment (sick or not sick?)
Risk of bleeding (Hx cancer, hx brain mass, ever had stroke, CT scan, Any surgeries, bleeding now?, blood transfusions? LOC/head injury?); want to know if you can give tpa when they decompensate
Get an echo (regardless of presentation); extension of physical exam
Basically 3 treatment options to REMOVE clot and immediately decrease PVR in massive PE
Systemic lysis
Catheter directed lysis
ECMO/surgical thrombectomy
Can also use NO for PVR decrease
The PVR increase in PE is not all about mechanical obstruction
This is why you can perform a pneumonectomy without significant increase in PVR (high elastance bed)
Clot burden causes release of all kinds of nasty vasoconstrictive substances
Intubation
CAUTION; can kill patient easily
Intubation/positive pressor has terrible hemodynamic effects
RSI meds = vasodilation, hypotension (use cardiostable induction meds like etomidate/ketamine)
acute preload reduction to RV
Positive pressure influence on PVR (see below)
But, also hypoxia and acedemia increase PVR; there is a balance
Pre-intubation art line is great
Inhaled NO at bedside
Consider starting pressor pre-intubation
Once on vent, aim for normoxia, normocapnea, low tidal volumes, 'sweet spot' of lung recruitment
Take home: if they look like they need to be intubated, they may need to go straight to thrombolysis
-Goal 2: Increase systemic BP
Why? want to improve coronary perfusion to RV. See perfusion pressure above
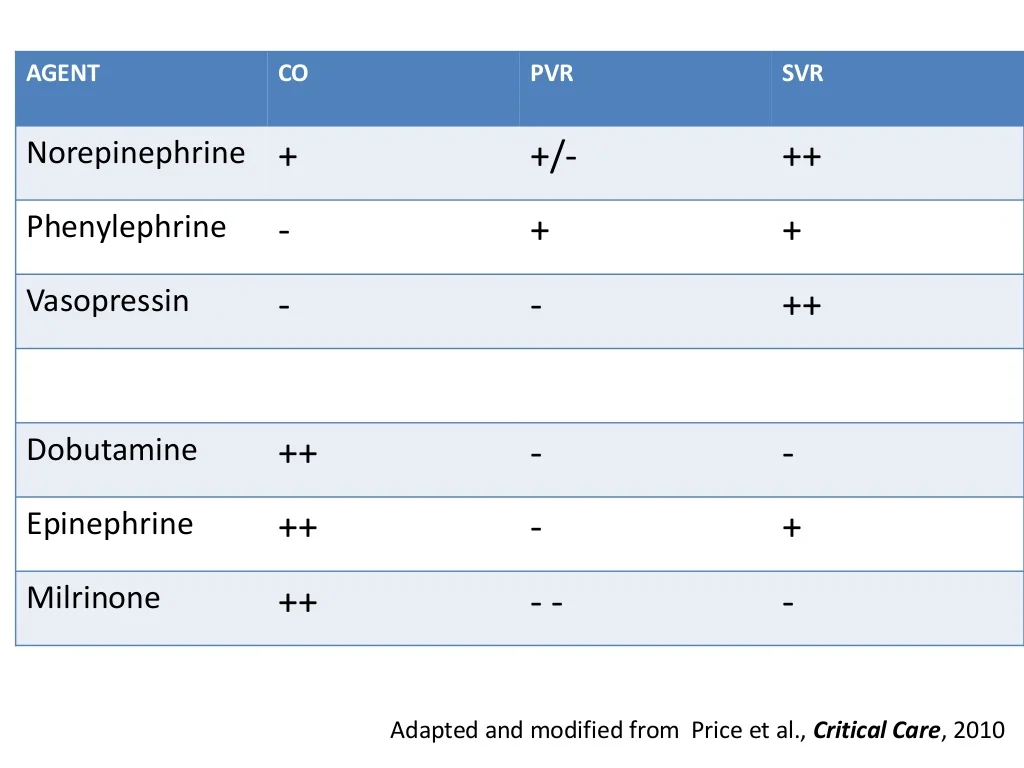
Use these in order (controversial, only validated in animal studies):
Norepi (Both neo and levo have increase in systemic BP, but levo has MUCH better effects on cardiac output and increased myocardial blood flow in animal study PE, maybe via B1 effects, or maybe neo is also raising PVR)
Vaso
Phenylephrine (may end up net even 2/2 increases in SVR and PVR, though PVR much less sensitive)
-Goal 3: Improve contractility of RV/preload
Not necessarily 'give more fluid;' may actually be harmful/worsen LV filling
From Yarborough trial, SMALL amount of fluid MIGHT be helpful; but use caution (like <500cc)
Inotropes (in order)
Dobutamine
Epinephrine
Milrinone
**usually grab levo, then dobutamine. If you need a second vasopressor, grab vasopressin. Vaso doesn't have much titratability.
Last resort: VA ECMO
Excellent decompression of RV
Some centers do this first as bridge to more definitive therapy
MOPETT Trial
Half-dose alteplase led to a marked reduction in pulmonary hypertension without sig. complications
Summary
Lytics Guidelines (AHA)
Anticoagulation
Anticoagulate with LMWH, IV/Sub-Q UFH, or fondaparinux (IA)
While working up PE, if pretest is moderate or high, and there are no contra-indications, start anticoagulation during the work-up (IC)
Fibrinolytics
Definition of Massive PE -Acute PE with sustained hypotension (systolic blood pressure <90 mm Hg for at least 15 minutes or requiring inotropic support, not due to a cause other than PE, such as arrhythmia, hypovolemia, sepsis, or left ventricular [LV] dysfunction), pulselessness, or persistent profound bradycardia (heart rate <40 bpm with signs or symptoms of shock).
Definition of Submassive PE -Acute PE without systemic hypotension (systolic blood pressure >90 mm Hg) but with either RV dysfunction or myocardial necrosis.
RV dysfunction means the presence of at least 1 of the following:
—RV dilation (apical 4-chamber RV diameter divided by LV diameter >0.9) or RV systolic dysfunction on echocardiography
—RV dilation (4-chamber RV diameter divided by LV diameter >0.9) on CT
—Elevation of BNP (>90 pg/mL)
—Elevation of N-terminal pro-BNP (>500 pg/mL); or
—Electrocardiographic changes (new complete or incomplete right bundle-branch block, anteroseptal ST elevation or depression, or anteroseptal T-wave inversion)
Myocardial necrosis is defined as either of the following:
—Elevation of troponin I (>0.4 ng/mL) or
—Elevation of troponin T (>0.1 ng/mL)
Fibrinolysis is reasonable for pts with massive PE and acceptable risk of bleeding complications (IIa/B)
Fibrinolysis may be considered for pts with submassive PE judged to have clinical evidence of adverse prognosis (hemodynamic instability, worsening resp. insufficiency, severe RV dysfunction, or major myocardial necrosis) and low risk of bleeding complications (IIb/C)
Fibrinolysis is not recommended for patients with submassive PE with only mild dysfunction, i.e. low risk PEs (III/B)
Fibrinolysis is not recommended for undifferentiated cardiac arrest (III/B)
Interventional and Surgical Options
Either catheter embolectomy or surgical embolectomy can be considered depending on institutional and operator preference (IIa/C)
Either of these are reasonable if the pt is still unstable in massive PE after fibrinolysis (IIa/C)
Also reasonable in massive PE, if the pt has a contra-indication to lysis (IIa/C)
May be considered in lieu of fibrinolysis in patients with submassive PE and evidence of adverse prognosis (IIb/C)
Not recommended for pts with PE at low risk (III/C)
Contraindications to Fibrinolysis
Absolute contraindications include
any prior intracranial hemorrhage,
known structural intracranial cerebrovascular disease (eg, arteriovenous malformation),
known malignant intracranial neoplasm,
ischemic stroke within 3 months,
suspected aortic dissection,
active bleeding or bleeding diathesis,
recent surgery encroaching on the spinal canal or brain, and
recent significant closed-head or facial trauma with radiographic evidence of bony fracture or brain injury.
Relative contraindications include
age >75 years;
current use of anticoagulation;
pregnancy;
noncompressible vascular punctures;
traumatic or prolonged cardiopulmonary resuscitation (>10 minutes);
recent internal bleeding (within 2 to 4 weeks);
history of chronic, severe, and poorly controlled hypertension;
severe uncontrolled hypertension on presentation (systolic blood pressure >180 mm Hg or diastolic blood pressure >110 mm Hg);
dementia;
remote (>3 months) ischemic stroke; and
major surgery within 3 weeks.
Recent surgery, depending on the territory involved, and minor injuries, including minor head trauma due to syncope, are not necessarily barriers to fibrinolysis.
The clinician is in the best position to judge the relative merits of fibrinolysis on a case-by-case basis.
Further on who should get lytics
It is preferable to confirm the diagnosis of PE with imaging before fibrinolysis is initiated. When direct imaging is unavailable or unsafe because of the patient’s unstable condition, an alternative approach favors aggressive early management, including fibrinolysis, of the patient with sustained hypotension (systolic blood pressure <90 mm Hg for at least 15 minutes or requiring inotropic support, not clearly due to a cause other than PE) when there is a high clinical pretest probability of PE and RV dysfunction on bedside transthoracic echocardiography.We do not endorse the strategy of treating subjects with undifferentiated cardiac arrest with fibrinolysis, because this approach lacks clinical benefit.