Core Content: Shock
Shock – What Every Provider Must Know
Shock is not just a drop in blood pressure—it's a life-threatening cellular crisis. In this episode of Pulmcast, we break down what every clinician needs to know about shock. From real-world cases to essential pathophysiology, you’ll walk away with a clearer understanding of oxygen delivery, shock subtypes, and bedside management tips for any critical care environment.
What Is Shock?
Shock is defined as a failure of circulatory function leading to inadequate oxygen delivery to meet tissue demands. It represents a mismatch between oxygen delivery (DO₂) and consumption (VO₂).
At the cellular level, cells shift from aerobic to anaerobic metabolism → leading to lactate buildup and energy deficit.
If uncorrected, this cascade results in organ dysfunction and ultimately death.
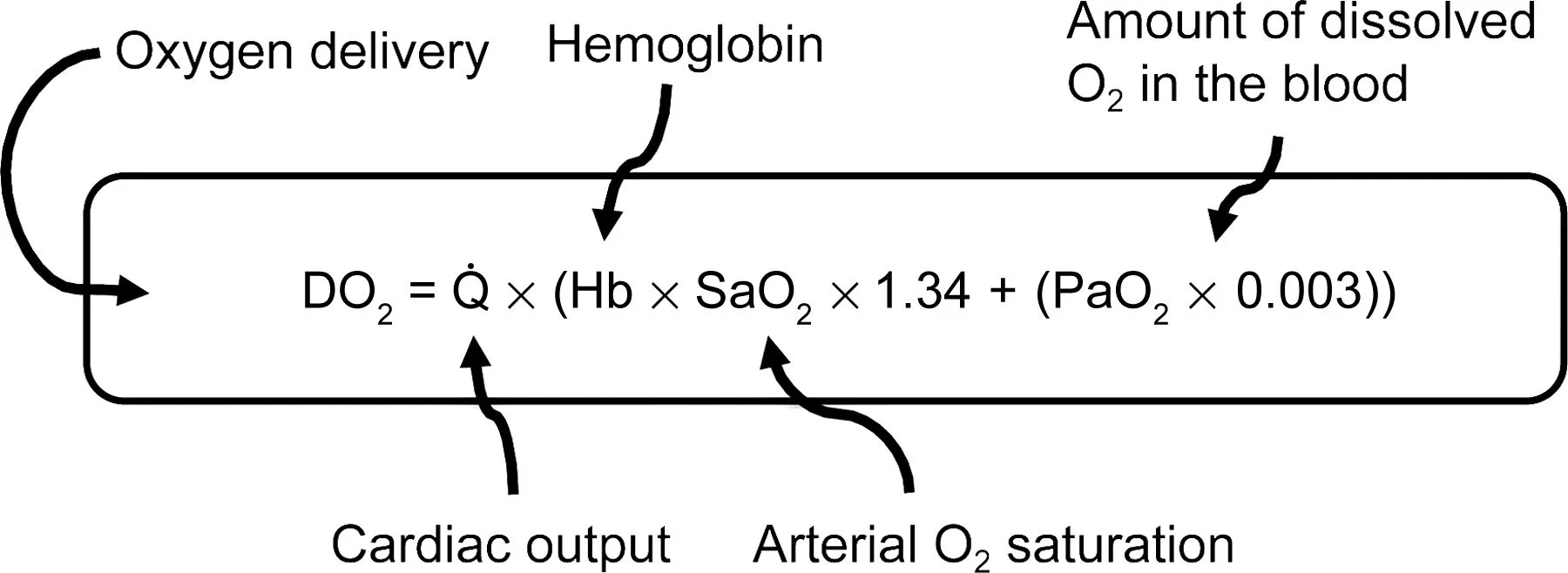
Key determinants of oxygen delivery (DO₂):
Cardiac output = Heart Rate × Stroke Volume
Arterial oxygen content = Hemoglobin × SpO₂ × (small contribution from PaO₂)
Arterial oxygen content (Arterial O2 sat + Hgb)
Cardiac output (HR x SV)
stroke volume determined by:
preload (how much blood is in the ventricle at the end of diastole)
afterload (or the force the heart has to pump against)
inotropy (how hard the heart is squeezing)
The Four Major Types of Shock
1. Distributive Shock
Primary Cause: Systemic vasodilation
Examples: Septic shock, anaphylaxis, neurogenic shock
Hemodynamics: ↓ SVR, ↑ or ↓ CO, normal preload
Case Insight: Normotensive septic patient with lactate >5.5 – always look beyond blood pressure!
Treatment:
IV fluids
Vasopressors (e.g., norepinephrine)
Inotropes if needed
Point-of-care ultrasound (POCUS) for volume status and cardiac function
2. Cardiogenic Shock
Primary Cause: Failure of the heart to pump effectively
Examples: MI, arrhythmias, myocarditis, valve failure
Hemodynamics: ↑ preload, ↓ CO, ↑ afterload
Case Insight: Pulmonary edema, JVD, hypotension → classic sick-heart profile
Treatment:
Non-invasive ventilation or intubation
Inotropes (e.g., dobutamine, milrinone)
Vasopressors only if needed to maintain MAP
Address the underlying cause: e.g., PCI, surgery
3. Obstructive Shock
Primary Cause: Mechanical obstruction to cardiac filling/output
Examples: PE, tamponade, tension pneumothorax
Hemodynamics: ↓ CO, ↑ SVR, variable preload
Case Insight: Post-op patient with McConnell’s sign → RV strain due to PE
Treatment:
Thrombolysis or thrombectomy (PE)
Pericardiocentesis (tamponade)
Needle decompression (pneumothorax) - check out our blog post on this
4. Hypovolemic Shock
Primary Cause: Loss of circulating volume
Examples: Hemorrhage, diarrhea, burns
Hemodynamics: ↓ preload, ↓ CO, ↑ SVR
Case Insight: Elderly patient with profuse diarrhea, dry mucosa, MAP 43
Treatment:
Replace lost volume with appropriate fluids
Use vasopressors early if MAP is dangerously low
Distinguish between hemorrhagic vs. non-hemorrhagic
Mixed Shock & Non-Response to Vasopressors
Patients may present with elements of multiple shock types
Always reassess when a patient isn’t responding to norepinephrine
Causes include:
Acidosis
Adrenal insufficiency
Hypocalcemia
Occult bleeding
Secondary shock subtype (e.g., obstructive + distributive)
Remember: The cognitive response to hypotension is NOT just “start another presser.”
DIAGNOSTIC PEARLS
Use the Shock Index = HR / SBP > 0.9 = occult shock
Bedside ultrasound is the great differentiator
RUSH exam (Rapid Ultrasound for Shock and Hypotension)
Look at IVC, cardiac function, lung sliding, free fluid
Shock Index Literature: https://www.ncbi.nlm.nih.gov/pubmed/23599863/
Occult Causes of non-response to vasopressors
Don't just place CVL and forget about it. http://rebelem.com/occult-causes-of-non-response-to-vasopressors/
Valuable tools:
POCUS
RUSH exam --> Rapid ultrasound in shock. Checking the pump, tank and pipes for causes of hypotension
Quick Takeaways
Shock = imbalance of DO₂ vs VO₂
4 Types: Distributive, Cardiogenic, Obstructive, Hypovolemic
Shock can occur even with a normal BP
Ultrasound is essential in early differentiation
Vasopressors are not a cure — treat the underlying cause
If you treat critically ill patients, understanding shock isn't optional—it’s vital.
Listen to the full episode on Pulmcast: Shock Core Content
Frequently Asked Questions (FAQ)
Shock is a critical condition where oxygen delivery fails to meet cellular demand, leading to organ dysfunction and, if uncorrected, death.
The major types of shock are distributive, cardiogenic, obstructive, and hypovolemic shock.
No. Patients can be in shock with normal blood pressure. Look for other signs such as lactic acidosis, poor perfusion, and altered mental status.
The Shock Index is calculated by dividing heart rate by systolic blood pressure. A value over 0.9 may suggest occult shock and the need for closer monitoring or intervention.
Bedside tools include point-of-care ultrasound (RUSH exam), lactate levels, perfusion markers, and clinical examination findings.
Attributions
“Small Steps" by Lee Rosevere is licensed under CC BY-NC 4.0 / Song has been cropped in length from original form
“Scary Ambient Music (Bloody House)” by TheBoseDeity is licensed under CC BY-NC 3.0 / Song has been cropped in length from original form
ICU Sounds by us
Cold Funk - Funkorama by Kevin MacLeod is licensed under a Creative Commons Attribution license (https://creativecommons.org/licenses/...)
Source: http://incompetech.com/music/royalty-...
Artist: http://incompetech.com/
Music promoted by Audio Library https://youtu.be/Vhd6Kc4TZls