How to write a note
In this page, we will be talking you through how to write a note using our templates. While the template may change depending on the billing/medical legal issues at the time, in general this is where you can find the information you need to input the note.
As a whole the first two thirds of the note is mainly filling out information. It is more mindless than the assessment and plan - you are putting information on the page. While you need to take note of this information, you are not coming up with it yourself - you are simply reading it, taking a curious note of it in your mind and spitting it back out on the page.
The last third of the note takes a little more ingenuity. This is where you are coming up with the assessment and plan yourself, and this is where your clinical skills come into play.
the beginning: Subjective, last 24 hours, hospital couse
This will vary based on the type of note your using (e.g. .glaconsult vs .glahistory vs .glaicunote), but in general at the very top you will have a basic “why are we taking care of this person” type statement. For consult notes, you will state who you were consulted by, and for progress notes you will have a subjective section which explains what has happened in the last 24 hours.
For all non-critical care notes (not charging CCT), you must include chief complaint here. The dotphrase is .glachiefcomplaint - this is for billing purposes, so it’s not super important that this is detailed. The billing people literally look at this to be able to correctly charge our note and as long as it is filled out it is all that matters.
The HPI (for a new note)
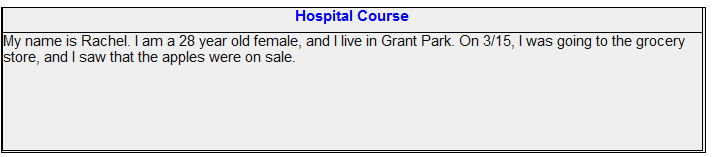
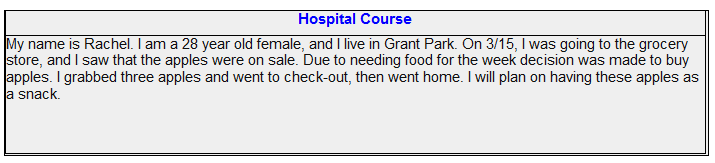
For the hospital course you will write a story about why the patient is here. If the patient has already been here and has been seen by our team, you can copy the the hospital course from the previous note (but ONLY if it was written by our team). You want this to be a full story from start to finish - almost act like you are explaining to a friend what has happened but in a more scientific, objective way. For example, if I were telling this story:
The ending is a bit abrupt, right? You would ask - and then what? It is INCOMPLETE. So you keep going and you would write -
Make sure to include why your patient was admitted, what happened when they got here, what happened when YOU got there, and their ultimate disposition.
The HPI (for an old note)
If the patient has been seen by our team you may copy their HPI over. In general, if you have time, you should try to improve it with new details, but if you don’t it’s okay too. But you can’t just copy it and leave it - in order to charge, you must have something new in the HPI (the billing people can see what you copied).
So how do we do that? Two ways. You will see people either add a sentence to the end of the old HPI, or you will see them skip a line and put a date. For example, if we were following my story from earlier, the highlighted text would be the new text you typed while everything else would be copied:
Each day you will put a new date and any updates. In general, these updates are a more concise version of the last 24 hour update above the HPI.
For past history, you literally just put however you got the history. You either reviewed it (below the section there is a med hx/etc) or you were unable to review it - usually people put that they were unable to review it due to encephalopathy or due to mechanical ventilation. This is also a billing thing, and it is important it is included every note.
the review of systems, the physical exam and the antibiotic table
For billing purposes, it is very important to include a fresh review of systems. More often than not unless the patient was on the vent or encephalopathic you will put the first option; where the three stars are (***), you can also put “as above”.
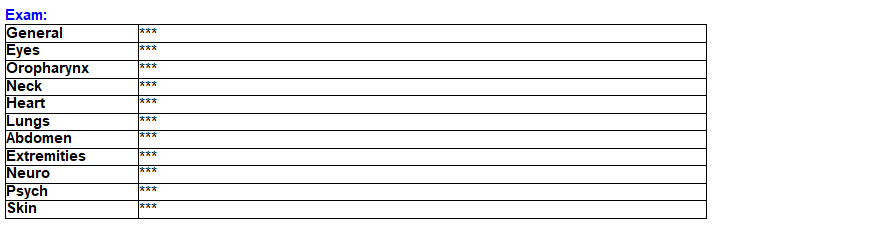
The Physical Exam
The physical exam is easy - it’s what it sounds like, a physical exam. There is common verbiage that people use (you will get used to this and see this often) but you put whatever you saw. Some common words you’ll see -
General: male/female in no acute distress, laying in bed, sitting in bed
Eyes: PERRL (pupils equal round and reactive to light), PER (pupils equal round and reactive), open, closed
Orophraynx: MMM (mucous membranes moist), mucous membranes dry, ETT in place, BiPAP mask in place
Neck: Supple (this means easily movable left, right, up and down - make sure to not blindly put this), trachea midline, obese
Heart: S1S2, fast rate, slow rate, irregularly irregular, murmurs if noted
Lungs: CTAB (clear to auscultation bilaterally), diminished, coarse, rhonchi, wheezes, rales
Abdomen: Soft, NTND (non-tender, non-distended), + BS (positive bowel sounds), obese
Extremities: + pulses, no edema, bilateral LE edema, pitting edema in legs, anasarca, thin, history of AKA/BKA
Neuro: AAO (alert and oriented), follows commands, equal strength, unequal strength, etc
Psych: Calm, agitated, anxious, unable to assess (with ventilated patients)
Skin: warm and dry, cool and dry, diaphoretic, surgical site c/d/i (clean dry and intact)
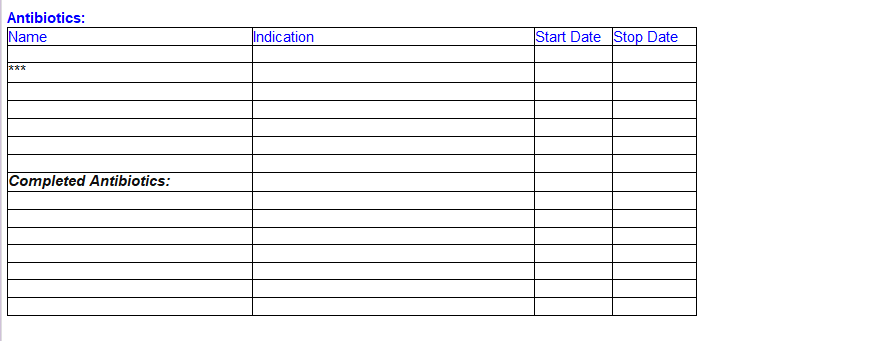
The Antibiotic Table
This is really important for us, but it’s not as important for billing. There are multiple ways to figure out/confirm what antibiotics they are on.
The Infectious Disease Box
One of the most common ways is to look for the infectious disease table. This is under the patient overview; it will list what meds are ordered and when they were last given. In this case, the patient was given cefepime, flagyl, xifaxan, vanc. The issue is you don’t know the start and stop dates. Because of that my preferred way of seeing the antibiotics is through the fever tab.
Fever Tab
The fever tab is great. When you are in overview, you can either type fever into the white box on the very right (where it says “Fever” on image) or click fever if it is saved on your tabs. With this, you can clearly see a list of abx and when they were given. in this patients case, they got:
Cefepime 3/15
Levaquin 3/14
Flagyl 3/14-3/16
Vanco 3/14-3/15 (changed doses)
The hard part is you can’t see what medications are active and what medications have been discontinued - so often I’ll look at this first, then look at the the infectious disease box to confirm what medications are active. Xifaxan is not on this because it is typically not used to treat infections, it is used for liver failure.
Med History Tab
If you’re really confused or someone has a really complex history (and you have a LOT of time) you can also go to the med history tab. Unfortunately with this you have to scroll through all the meds and it takes much longer; but you can get much more detailed info. You can see under the medication name there is a indication of use (although people don’t always put this) and start/end date.
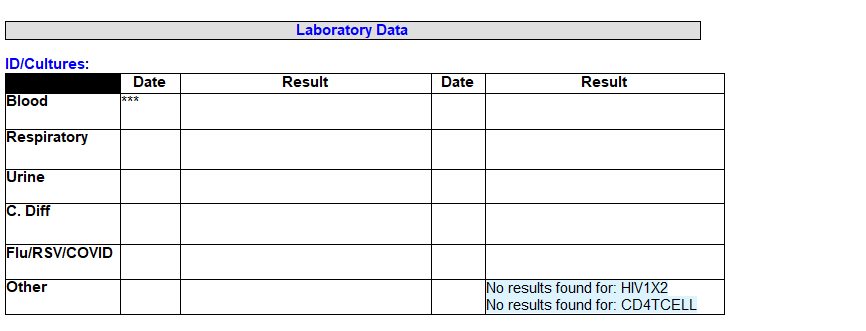
The Laboratory Data and Data/Imaging Table
To find your culture data, you’re going to want to look under the “Micro” tab under summary. This will show any kind of microbiology data in the last 21 days. What’s nice with this tab is everything that is bad is in red. If a procedure says “no result” it means it actually wasn’t drawn (in this case, the adult blood cultures were drawn from one bottle but the other bottle was never drawn). You will put the date it was drawn (NOT the date it was updated) and the result. Sometimes you’ll see people write it as “NG x 3 days” (no growth for three days) or “NGTD” (no growth to date).
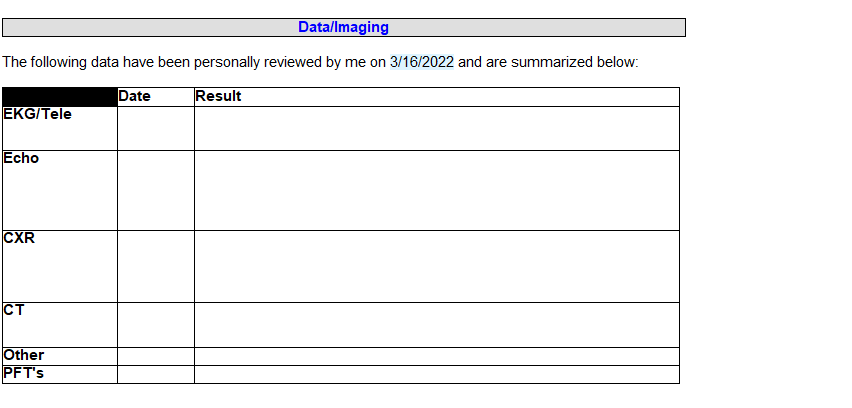
The Data/Imaging Table
EKG/Tele: For this section you will put either what is on the patients telemetry (e.g. they’re in the ICU - what is their heart rate on the monitor) or what you saw on their previous EKG. For this, you will usually put their heart rhythm (SR, Afib, etc) and if you want you can put the general rate (e.g. SR 90s, ST 100s). For the date, you can type “.todaydate” to automatically pull up todays date.
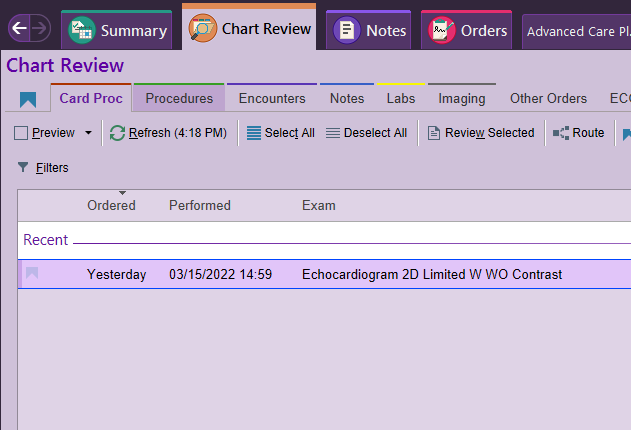
Echo: you want to put their most recent echocardiogram results, even if it wasn’t from this admission. To find the patients echo information (or any cardiac procedures - e.g. vascular ultrasounds, previous RHC/LHC) you will go to Chart Review —> Card Proc. Here it will list all the previous echos - either limited or complete. Make sure you look for transTHORACIC echo (via the skin) versus transESOPHAGEAL echos (TEE - in the esophagus).
Other: Here you can put either other cardiac procedures (like vascular procedures - ultrasounds, etc), MRIs, whatever you want really.
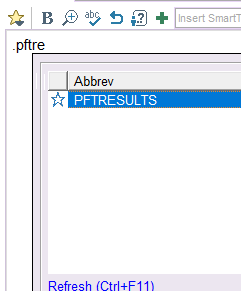
PFTs: being a pulmonary/critical care group, we love our PFTs. There are two ways you can find PFTs -
Type “.pftresults” while you are in a note, and it will pull up whatever PFTs it can find in EPIC. In order for this to work it has to be logged correctly in the system; if this doesn’t work it doesn’t necessarily mean the patient doesn’t have them
Click the magnifying glass next to EpicCare on the top right of your screen (next to your name) and type “Pulmonary Function”
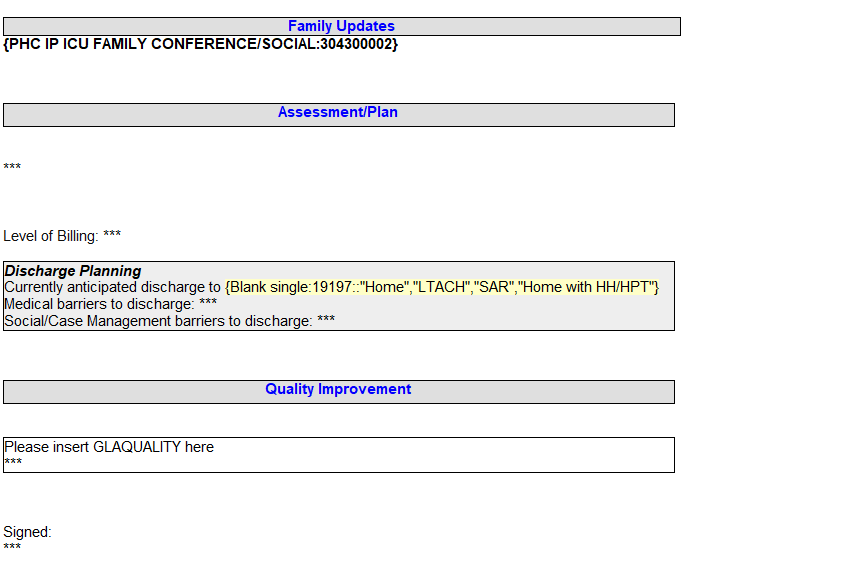
Family Updates, assessment plan, Quality Improvement
Family Updates: For family updates, you write whether you updated the family or not. You can also put you are going to update the family on arrival; that the primary team will update the family; etc. This is where you can also have code status discussions, etc. A nice touch is to add “.todaydate” at the end to put an official date on your conversation.
Assessment/Plan: Here’s where you do all the clinical work and write your assessment and plan.
Discharge Planning: This has nothing to do with billing, it was done to help our case management team. Fill it out as best you can.
Quality Improvement: highlight the entire table and type “.glaquality”. A table will pop up. Fill out the table with all the information directed.