Blood Product Utilization in the ICU: Evidence-Based Transfusion Strategies
Why Blood Product Utilization Matters in Critical Care
Blood products save lives—but they are not benign. In the ICU, inappropriate transfusion increases the risk of TRALI, TACO, infection, immunomodulation, electrolyte disturbances, and mortality. Modern critical care emphasizes restrictive, targeted, and physiology-driven transfusion strategies, supported by large randomized trials and viscoelastic testing.
This guide breaks down when to transfuse, what to transfuse, and how to transfuse—grounded in evidence and practical bedside decision-making.
Packed Red Blood Cells (PRBCs)
Physiologic Role
PRBCs increase oxygen delivery by raising hemoglobin concentration. However, increasing hemoglobin does not automatically improve tissue oxygen utilization, especially in sepsis or critical illness.
Evidence-Based Transfusion Thresholds
Restrictive transfusion is standard of care in most ICU patients.
| Clinical Scenario | Recommended Transfusion Threshold |
|---|---|
| General critically ill ICU patients | Hemoglobin < 7 g/dL |
| Septic shock | Hemoglobin < 7 g/dL |
| Acute coronary syndrome / myocardial ischemia | Hemoglobin < 8 g/dL |
| Active hemorrhage with hemodynamic instability | Transfuse based on physiology and shock state |
One unit of PRBCs raises hemoglobin by ~1 g/dL and hematocrit by ~3% (if no ongoing bleeding).
Key trials: TRICC, TRISS, CHEST, MINT
Fresh Frozen Plasma (FFP)
What FFP Does
FFP contains all coagulation factors and provides both hemostatic support and intravascular volume expansion.
Indications for FFP
Active bleeding with suspected or known coagulopathy
Massive transfusion–associated dilutional coagulopathy
Liver disease with impaired hemostasis
DIC with bleeding
Urgent invasive procedures with coagulopathy
Warfarin reversal with active bleeding (often with PCC)
Target Parameters
INR < 2
PT < 18 sec
PTT < 35 sec
Patients with higher baseline INR derive the greatest correction from FFP. One unit of FFP has an INR of ~1.3.
Cryoprecipitate (Cryo)
What Cryo Replaces
Cryoprecipitate is concentrated fibrinogen and factor replacement:
Fibrinogen
Factor VIII
Factor XIII
von Willebrand factor
When to Use Cryo
Hypofibrinogenemia with bleeding
Massive transfusion protocols
DIC or liver disease with low fibrinogen
Practical Thresholds
| Laboratory Findings | Recommended Therapy |
|---|---|
| Fibrinogen < 50 mg/dL | Fresh Frozen Plasma + Cryoprecipitate |
| Fibrinogen < 100 mg/dL | Cryoprecipitate until fibrinogen > 200 mg/dL |
| Fibrinogen > 100 mg/dL with elevated PT/PTT | Fresh Frozen Plasma |
A 10‑unit pool raises fibrinogen ~70 mg/dL with minimal volume.
⚠️ Cryo does not reverse warfarin or DOACs.
Platelet Transfusion in the ICU
Platelet Thresholds
| Clinical Context | Platelet Transfusion Threshold |
|---|---|
| Prophylaxis (no active bleeding) | < 10,000 / µL |
| Active bleeding or prior to invasive procedure | < 50,000 / µL |
| CNS injury, neurosurgery, or intrathecal catheter | < 100,000 / µL |
Each apheresis unit increases platelets by ~30,000 within minutes.
Special Populations (Use With Caution)
Platelet transfusion may worsen outcomes unless bleeding is life‑threatening:
HIT
TTP / HUS
ITP
DIC
Links:
NEJM Platelet Transfusion Before CVC – https://www.nejm.org/doi/full/10.1056/NEJMoa2214322
Complications of Blood Product Transfusion
TRALI: Acute hypoxemic respiratory failure within 6 hours
TACO: Volume overload, especially in elderly or heart failure
Hypocalcemia: Citrate binding → treat with calcium
Hyperkalemia: Stored RBC potassium leak
Hypothermia: Use blood warmers during massive transfusion
Calcium replacement:
1 g calcium gluconate per 2 units PRBCs
Use calcium chloride in liver dysfunction
Prothrombin Complex Concentrates (PCCs)
K‑Centra
Factors II, VII, IX, X
Warfarin reversal with vitamin K
Dose: 25–50 units/kg
Profilnine
Factors II, IX, X (no VII)
Give with vitamin K ± FFP
⚠️ PCCs are prothrombotic—use only when benefit outweighs risk.
Antifibrinolytics
Tranexamic Acid (TXA)
Trauma hemorrhage: 1 g bolus → 1 g over 8 hours
Postpartum hemorrhage: 1 g IV within 3 hours
tPA‑associated ICH: 10–15 mg/kg
Links:
CRASH‑2 / PATCH Trauma – https://www.nejm.org/doi/full/10.1056/NEJMoa2215457
Aminocaproic Acid (Amicar)
Severe thrombocytopenia bleeding
ECMO‑associated hemorrhage
Anticoagulation Reversal Cheat Sheet
| Anticoagulant | Primary Reversal Agent |
|---|---|
| Unfractionated Heparin | Protamine sulfate |
| Low Molecular Weight Heparin (Enoxaparin) | Protamine (partial reversal) |
| Warfarin | Vitamin K + Prothrombin Complex Concentrate (PCC) |
| Dabigatran (Pradaxa) | Idarucizumab (Praxbind) |
| Factor Xa inhibitors (Apixaban, Rivaroxaban) | Andexanet alfa (Andexxa) |
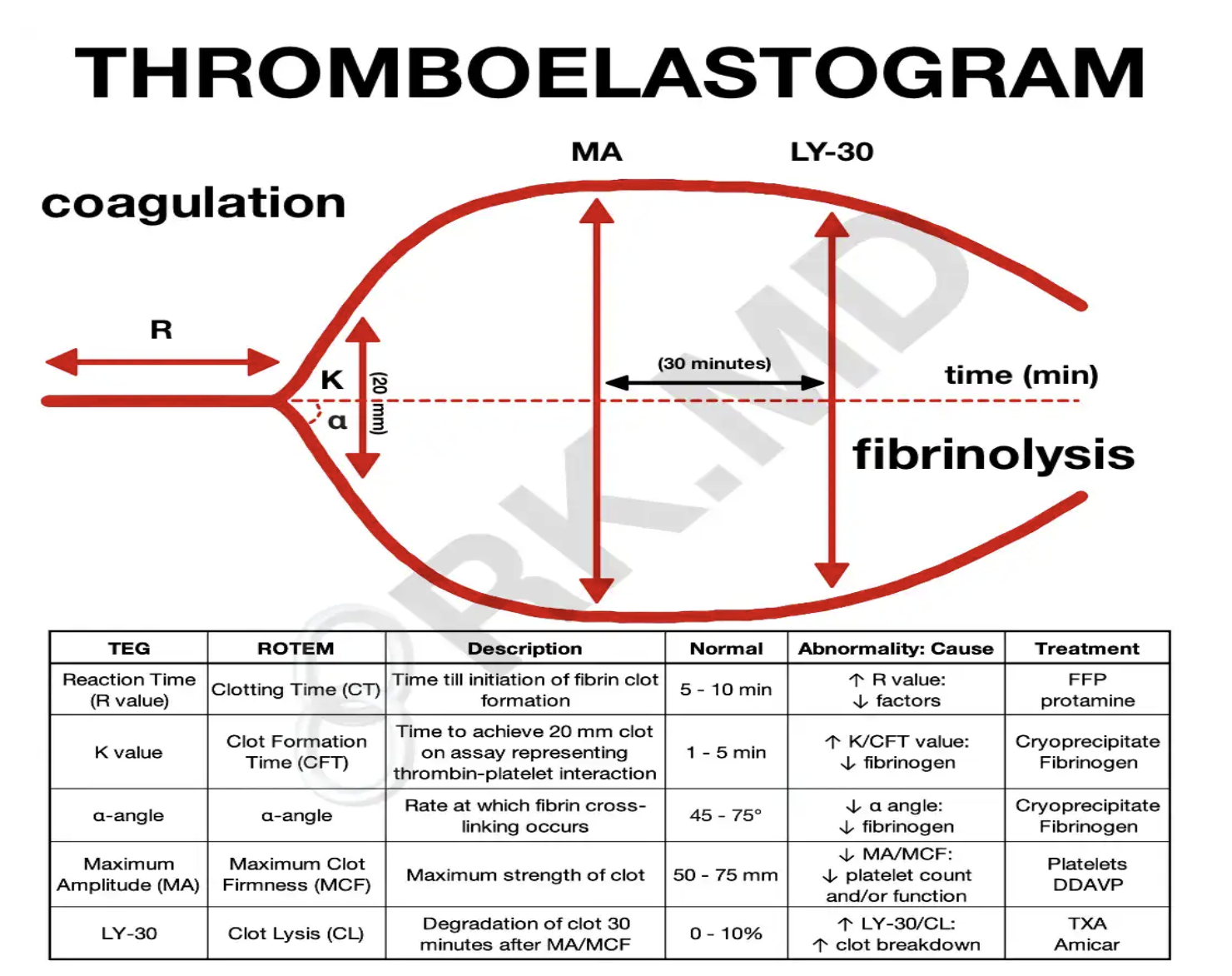
TEG‑Guided Transfusion: Precision Over Guesswork
Thromboelastography evaluates clot formation, strength, and breakdown in real time.
| TEG Finding | Physiologic Interpretation | Targeted Treatment |
|---|---|---|
| Prolonged R-time | Clotting factor deficiency | FFP or Prothrombin Complex Concentrate |
| Low alpha angle or prolonged K-time | Low fibrinogen | Cryoprecipitate |
| Low Maximum Amplitude (MA) | Platelet dysfunction or thrombocytopenia | Platelet transfusion or DDAVP |
| Elevated LY30 | Hyperfibrinolysis | Tranexamic acid or Aminocaproic acid |
Benefits:
Reduces unnecessary transfusions
Improves targeted resuscitation in trauma, liver disease, cardiac surgery
Links:
JTH TEG Review – https://onlinelibrary.wiley.com/doi/full/10.1111/jth.14447
Key Takeaways for ICU Practice
Restrictive transfusion saves lives
Treat physiology, not just lab values
Use Cryo for fibrinogen, not FFP
Platelets are not benign—know when not to transfuse
TEG enables precision resuscitation
Want More ICU Pearls?
Explore evidence-based critical care education at Pulmcast:
Blog: https://www.pulmcast.com
Instagram: https://www.instagram.com/pulmcast