Dr. Ultrasound and Mr. Hyde: my confessions as an educator and ICU geek
John Heisler, PA-C
“I wish I were better at ultrasound.”
”I’m not as good at ultrasound as people on my team.”
”I keep meaning to practice scanning on shift, but there are so many other things I could be doing.”
Let's Be Honest
I think most people in our field have had some or all of these thoughts. I feel guilty thinking them and certainly have a hard time verbalizing to other team members. Point of Care Ultrasound (POCUS) has swept the medical world over the last few years, particularly in Emergency Medicine and Critical Care. It is even now being incorporated into Internal Medicine residencies and will be ubiquitous in most specialties within a few years, especially as the pocket US technology gets better and cheaper. 4
Ultrasound has a lot of utility, and our program felt it valuable enough to invest in a 2 day course for all of us to attend. We all talk about using ultrasound frequently, but I'd venture to guess the percentage of providers who use it on a daily basis in our practice is under 50%, and may be much lower than that. As a consequence of not using it routinely, our skills from the course have decayed, it takes us longer to get views (if we can get good views at all), and our skills at interpreting what we are seeing are such that we don't trust it enough to make clinical judgments.2
“We all talk about using ultrasound frequently, but I’d venture to guess the percentage of providers who use it on a daily basis in our practice is under 50%”
The Learning Curve
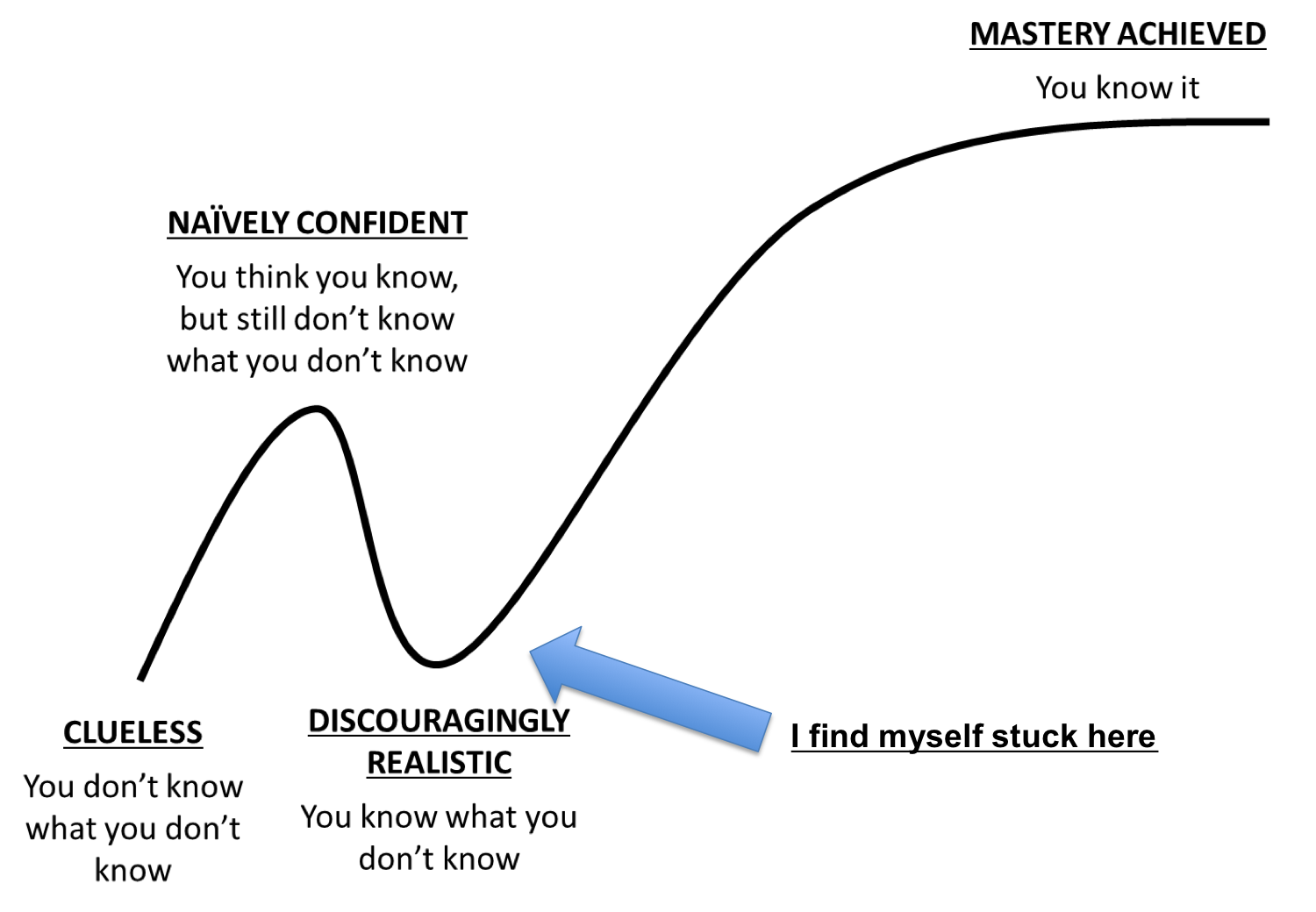
We have perpetuated the learning curve and kept it firmly in place. It becomes a vicious cycle. We don't scan because it takes us longer than expected, and it is low yield because we are out of practice. We get more out of practice the less we use ultrasound.
It's tough to see colleagues pass me by, so I've decided to make POCUS a priority and make time to scan. I've started going through the Ultrasound modules our program has purchased like I should have several months ago, I've been listening to Ultrasound Podcast by Mike and Matt (those guys are hilarious).1 I've committed to scanning at least a few times per shift. I can already see myself getting faster.
Just a few weeks ago, one of our colleagues discovered tamponade physiology and facilitated emergent pericardiocentesis at bedside- POCUS matters.
"But we have a million things on shift to do," you say?
Of course we do, and that's not going to change. But POCUS isn't going away. It's probably more important than a lot of the other things we make time to do on shift. Making it a priority will make you faster, getting views will be easy, you will be able to quickly interpret what you are looking at, and eventually you will be able to make clinical decisions based on it.
“Pocus isn’t going away”
I've definitely noticed myself using it more on night shift- particularly if we have a night with fewer admissions. I've got to make it enough of a priority that I find the time during a typical day shift too. To quote Mike and Matt "Ultrasound is a skill like everything else, you get better as you practice."
Pitfalls
Common Mistakes and Downsides: Despite all the utility, there are some downsides to ultrasound. 1,2
1 - Measure of fluid responsiveness: Ultrasound has its challenges here just like the other modalities we've historically used to measure fluid responsiveness. Although not useless in patients on positive pressure, IVC assessment can be skewed by respiratory effort, portion of the IVC you are looking at, and disease states like pulmonary hypertension. Tachycardia can make the LV appear hyperdynamic to the untrained eye while bradycardia can make the cardiac output seem artificially low. It's certainly not perfect, and there are many caveats to its accuracy. If you continue to gain experience with ultrasound, it's another tool in your toolbox. For our colleagues on the team who practice at sites with fewer resources and less specialty coverage, it is perhaps even more important to be proficient with US.
2 - Jumping to conclusions: Inexperienced ultrasound clinicians can misinterpret images, potentially prompting incorrect clinical decisions. How can you prevent this as a new user? Scan with someone more experienced than you. Practice getting windows on your own, make a decision on what you think you see, and run it by the team. Know that you are new and take your findings with a grain of salt- especially if they contradict your other findings.
Each time you pick up the probe, have a question you want to answer- don't scan just to scan. Ask yourself: What do I want to know about this patient? Will this assist in determining what type of shock they are in? Is this to assess volume status? Can I rule out PTX? If you scan with a question in mind, you won't get distracted, and you can start to assess whether your views and findings allowed you to answer your clinical questions. It's ok if you can't answer those questions at first. Keep practicing and talking to your colleagues with more ultrasound experience. That's how you'll improve!
The human mind loves to jump to conclusions. Be careful to put anything you find on ultrasound into the clinical context of the patient and verify any abnormal findings with an experienced provider.
3 - Not being methodical: As with any new skill, have a reproducible process that you use each time to ensure you get all aspects and views of what you are scanning. For example, when evaluating the heart, go through every view, every time. You will develop a process, and you are less likely to make a decision on incomplete information.
How can we guard against these mistakes?
- Have a clinical question
- Seek images that can answer your question
- Know your own limitations
- Undergo Ultrasound Training
- Review your findings with a more experienced clinician
So I convinced you and now you'd like to renew your interest in ultrasound and get better right?
If you are a member of our group, you have access to an ultrasound module we purchased which has modules on anything and everything (cardiac, lung, procedural, FAST/RUSH exams, abdominal, and a lot more.)
We are also partnering with the Department of Echo at the system level to develop a credentialing process for POCUS. There will bededicated time on shift with trained ultrasonographers to learn how to acquire desired images. Once we have completed that aspect of the training, an experienced provider will review a number of your images and ensure you are obtaining and interpreting your views correctly. The system goal is to have an echo certified cardiologist help you interpret your findings if it's essential to the care of your critically ill patient 24/7. The cardiologist will be able to view your bedside scans directly in EMR and help interpret them. That's the future folks, and it's coming sooner than you think.
I think it's time that ultrasound moves from just an interesting novelty to become a cornerstone of daily practice in the ICU. Who is with me?
“I think it’s time that ultrasound moves from just an interesting novelty to become a cornerstone of daily practice in the ICU. ”
Wrapping Up
Different opinion? Have more to say on this topic? Please leave your comments below, because we would love to hear from you.
As Jer says, Until next time...keep breathing, keep streaming, and keep reading.
References:
The Ultrasound Podcast
- [http://www.ultrasoundpodcast.com/2014/03/mistakes/][0]
- [http://www.ultrasoundpodcast.com/2013/04/the-future-or-medical-education-and-some-lung-ultrasound-foamed/][1]
- [http://www.ultrasoundpodcast.com/2013/05/future-of-medical-education-part-2-a-little-bit-of-lung-ultrasound-and-an-all-new-ultrasound-ibook-foamed/][2]
KeyLime Podcast
4 Internal Medicine Residents Using Pocket US[https://poddirectory.com/episode/7104867/84-pocket-sized-ultrasound][3]
Pocket-sized ultrasound as an aid to physical diagnosis for internal medicine residents: a randomized trial. Journal of General Internal Medicine. 2015 Feb; 30(2):199-206.