Swan-Ganz Catheters
Dr. Werner Frossman (at 25 years old!) was a German physician/cardiology intern who went against the norm and placed a catheter in his own heart on August 29, 1929; after placing the catheter via the antecubital vein under fluoroscopy, he climbed two flights of stairs and got an x-ray proving it was in the right atrium, all with a catheter dangling from his arm
He got in severe trouble for this and had to give up cardiology; became a urologist. Later in 1956, he won the Nobel Prize in medicine for his work
Right heart catheterization became a valuable tool for measuring hemodynamics, gas exchange and heart-lung interaction; but it all required fluoroscopic assistance and marked technical skill for correct placement, and had to be done in the cath lab
Dr. Jeremy Swan was watching sailboats in Santa Monica Bay during an outing with his children and he came up with the idea of a flow directed catheter - he postulated a small balloon would act as sail/parachute by catching blood flow, increasing the ease and frequency of passage (you can do it at bedside!!)
In 1970 Dr. Swan, with the held of his friend Dr. Ganz, created a a balloon tipped flow directed pulmonary artery catheter (PAC) that became accepted widely as a bedside tool for hemodynamic measurements
In 2016, Wheeler et. al. concluded in a RCT that PAC guided therapy did not improve survival or organ function but DID have more complications when compared to CVL guided therapy - which is why we don’t see it in every one of our patients
It is similar to a CVL except a balloon at the end of the catheter is inflated with ~1.5cc of air, which allows it to “float” through the right side of the heart and “wedge” into a small branch of the pulmonary artery. You’ll often hear this called “floating a swan”
so.. what are you looking at when you float a swan?
hemodynamic values, specifically cardiac performance and adequacy of systemic oxygenation
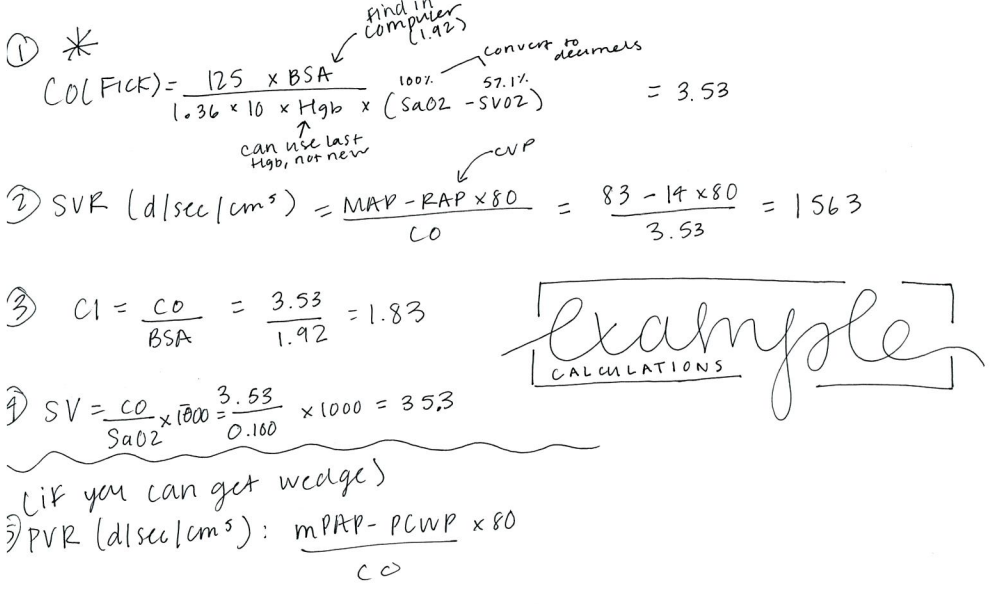
CO/CI: measured with thermodilution
Thermodilution: you take the difference in temps and put it in a graph to spit out a measurement (done on monitor in room)
PA Pressure - continuous measurement if your SGC is in correct placement (see below)
Pulmonary artery wedge pressure (PAWP)
You wedge balloon as below and get one measurement, then deflate balloon
CVP (RAP) - continuous measurement
Mixed venous O2 sat (SCVO2) -> unlike a central line, on a swan this will be continuous measurement
Waveforms
As you advance the balloon through the heart, you will see different waveforms on the monitor. First you’ll encounter the right atrium waveform (which will look like the waveform when you get CVP from CVL); you will advance the catheter and get a RV waveform; as you advance it further, you’ll get a PA waveform. This tells you you are in the pulmonary artery. At this point the balloon is not inflated. The nurse will then inflate the balloon and you advance forward until you see the the PA wedge waveform (very right). It is important that the BALLOON IS ONLY INFLATED when you are looking at the monitor.
Causes of elevated RAP
RV Infarction
pHTN
Pulmonic Stenosis
L —> R shunts
Tricuspid valvular disease
volume overload
Impaired RV contractile function
Causes of elevated PAP
Primary lung disease
Primary pHTN
PE
Hypoxemia w/pulm vasoconstriction
L —> R shunts
L heart failure (any cause)
Mitral valvular disease
Volume overload
Causes of Elevated PAWP
mitral stenosis
LV systolic dysfunction
Primary LV diastolic dysfunction
LV volume overload
Decr LV compliance
Normal Pressures
Right Atrial Pressure (CVP): 3-8 mmHg
RV Pressure: 15-30/3-8 mmHg
PA Pressure: 15-30/5-15 mmHg
PCWP: <15mmHg
CO: 4.5-8 L/min
CI: 2.5-4 L/min/m2
SvO2 >70%