PULMCAST AIRWAY TRACK
“In the ICU, a difficult airway isn’t just a procedural challenge - it’s a race against physiology. Success depends not just on skill, but on preparation, anticipation, and the calm execution of a well-rehearsed plan.” - Dr. Scott Weingart, MD, FCCM, Emergency and Critical Care Physician, EMCrit Podcast
Why Airway Management Matters in Critical Care
Mastering airway management is vital for every provider in the ICU. Effective airway control isn’t just technique - it’s about preparation, teamwork, and reducing harm when time is critical.
General Strategy & Airway Management Plan: A, B, C
Always be ready with your plan A, plan B and plan C. Use mneumonics like STOP MAID and LEMON (see lower on this page) to guide your prep and improve speed under pressure. Make this plan based on the issue you predict will happen.
Mnemonic for airway preparation: STOP MAID
General Recommended Approach for APP Intubations
KEY ASSESSMENT TOOLS
Difficult LMA = RODS
Restricted mouth opening
Obstruction
Distorted airway
Stiff lungs or c-spine
Difficult surgical airway = SHORT
Surgery
Hematoma
Obesity
Radiation distortion or other deformity
Tumor
Difficult intubation = LEMON
Look externally
Evaluate 3-3-2 rule
Mallampati score
Obstruction
Neck Mobility
Difficult BVM = BONES
Beard
Obese
No teeth
Elderly
Sleep Apnea / Snoring
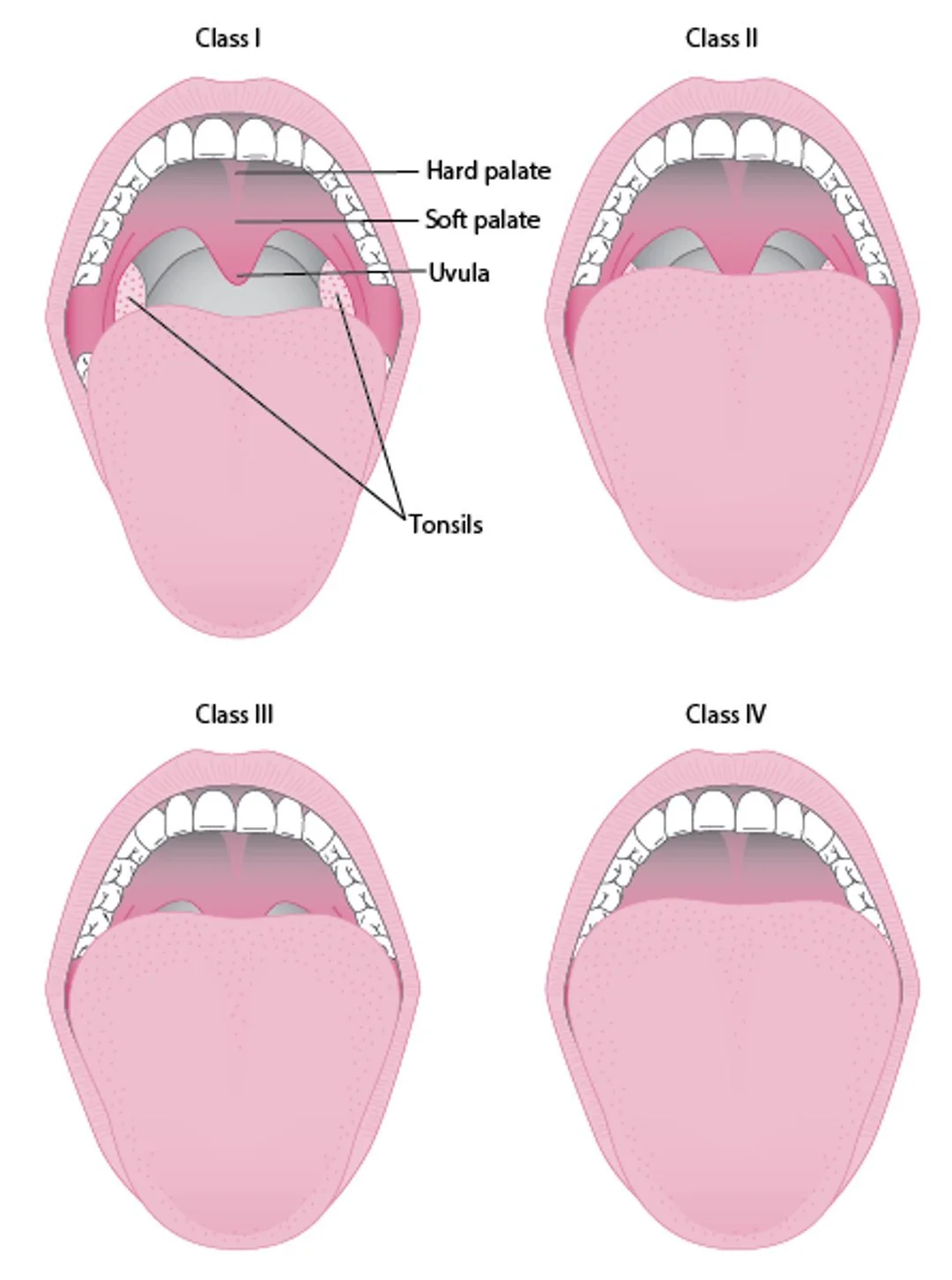
MALLAMPATI SCORE
The Mallampati score helps anticipate difficult visualization during intubation.
Class I: Soft palate, uvula, fauces, pillars visible
Class II: Soft palate, uvula, fauces visible
Class III: Soft palate, base of uvula visible
Class IV: Only hard palate visible
Cormack-Lehane Classification
Grade 1: Full view of glottis
Grade 2a: Partial view of glottis
Grade 2b: Only posterior extremity of glottis seen or only arytenoid cartilages
Grade 3: Only epiglottis seen, none of glottis seen
Grade 4: Neither glottis nor epiglottis seen
Airway Basics
Oxygenation
Further topics on Oxygenation
Delayed Sequence Intubation:
The Failed Airway
If the airway isn’t secured:
Declare “Failed Airway” immediately (sometimes the hardest part!)
Shift focus to oxygenation strategies (e.g. mask ventilation, supraglottic airway)
Perform emergent cricothyrotomy using the scapel-finger-bougie method for CICO (can’t intubate, can’t oxygenate)
LMA Insertion
Cricothyrotomy
If true can't intubate, can't oxygenate (CICO), emergent cricothyrotomy should be performed. We prefer the scalpel-finger-bougie technique.
Real, Live Cric
Emcrit on the Surgical Airway
Miscellaneous
Use of the Bougie
LaMW: Intubating the Hypotensive Patient
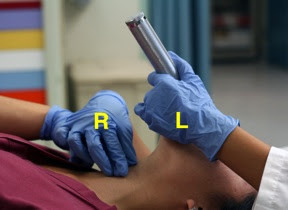
BURP Maneuver
The "BURP Maneuver" of Backwards Upwards Rightwards Pressure aka Bimanual Laryngoscopy. It is pressure applied to the thyroid cartilage of the upper Adam's Apple and not the cricoid cartilage. It reverses the distorting forces of the laryngoscope's lift, and can optimize the view of the notorious "Anterior Larynx."
POCPOM Maneuver
POCPOM or Pull Out Cheek - Push On Maxilla manuever is used when the intubator is hampered by a crowded oral cavity: small mouth or limited mouth opening due to arthritis, jaw trauma, TMJ problems, buck teeth; angioedema, tongue swelling, etc.
Bed Up - Head Elevated (BUHE)
BUHE or Bed Up Head Elevated is the optimal position for pre-oxygenation and induction of morbidly obese patients. The head up position maximizes view during direct laryngoscopy, while the bed elevation increases chest wall compliance to facilitate BMV.
BUHE may even be beneficial for all airways if feasible. See BUHE Video and this article: Head-Elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit.